Alberta Governor's Newsletter December 2019

-
In this Issue:
- GOVERNOR’S MESSAGE
- CALENDAR OF EVENTS
- PATERNAL ADVICE TO YOUNG INTERNISTS BEGINNING A TEACHING CAREER
- EXCELLENT TOOLS AND RESOURCES FOR MEMBERS
- ACP AS ADVOCATE
- FACP – BECOME ONE TODAY!
- WELCOME TO NEW MEMBERS
- GET INVOLVED IN YOUR CHAPTER!

Peter G Hamilton, MBBCh, FACP, ACP Governor
GOVERNOR’S MESSAGE
Thanks to the hard work of Dr. Lee-Ann Hawkins, Dr. Rahim Kachra and the planning committee, we celebrated a very successful conference in internal medicine. There were 190 registrants for the Rocky Mountain/ACP Western Canada Chapters Annual Meeting, from over twenty cities, six provinces, three US states and three countries.
Dr. Robert Herman delivered the inaugural R.J. Herman Plenary lecture. He reminisced on the journey that the Rocky Mountain Meeting had taken since its inception. Although it went through a rocky time, thanks in large part to Bob the meeting has survived and gone from strength to strength.
The A.M. Edwards lecture was given by Dr. Anita Palepu, Head of the Department of Medicine at UBC. She reflected on the challenges that internists face when dealing with complex care. Dr. Edwards (Buzz), a previous Governor of the Alberta Chapter, was one of the founding members of the ACP Advances in Medicine meeting that was held in Banff from the mid 1960's to the early 1990's. Buzz died suddenly on May 5, 1999 while attending cardiology rounds. I share my diary entry from that day:
“We all come and go on this journey called life, some before others. It is for this day that we must all prepare, for no tomorrows are guaranteed and all must succumb. Sadly, we will all, soon be forgotten, like a stone thrown into a small pond. The bigger stone makes a bigger ripple but soon, it too is still.”
The meeting also boasted 16 outstanding workshops, covering everything from immunology for the internist to mindful practice and financial planning. Dr. Jeff Schaefer did a stellar job of entertaining us with Medical Jeopardy, with the winners from UBC. A big thank you to the faculty, the organizing committee, the sponsors and the University of Calgary.
Save the date for next year's annual meeting November 19-21, 2020 in Banff.
I am proud to announce that the Alberta Chapter has once again received an ACP Chapter Excellence Award!
Congratulations to Dr. Neil Gibson for being the recipient the ACP Alberta Chapter Laureate Award for Distinguished Service.

(L-R): Dr. Bert Govig (Governor, Quebec Chapter); Dr. Neil Gibson (former Governor, Alberta Chapter); Dr. Robert McLean (ACP President)
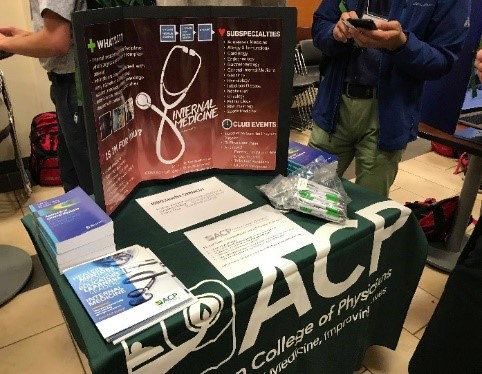
A big thank you goes out to the student members of the ACP who participated in the Clubs Fair for first year MD students. It was a resounding success with many signing up as student members of the ACP. To encourage participation, they held a raffle for five copies of the textbook “Approach to Internal Medicine.”
One of our distinguished clinicians, Dr. Arnie Voth, has submitted an insightful article (see below). I hope that there will be more to come, and I encourage all members to contribute to the newsletter.

Dr. Voth (centre) with Dr.Rolfson (left) and Dr. Ballermann at the Chairs Annual Dinner
At a time when we are reminded daily of the impact of anthropomorphic global warming it is surprising to hear so little discussion about the impact of over-population. Deborah Anderson from Boston University, School of Medicine, published an interesting editorial in the NEJM in which she advocates for a contraception revolution. She points out that the population of the world is at 7.7 billion and will reach 9 billion by 2050. The U.N. believes that the earth's carrying capacity has already been reached. At the same time, of the approximately 210 million pregnancies worldwide every year, at least 40% (80 million) are unintended. Over 222 million women in the world's poorest countries have no access to family planning. (To read the editorial go to, NEJM Aug 1, 2019)
I recently visited my alma mater at ‘WITS’, University of the Witwatersrand in Johannesburg, South Africa to celebrate the 100th anniversary of the medical school. The Dean of Medical Sciences, Dr. Martin Veller, is a friend and classmate. He gave me the opportunity to tour the medical school and compare notes about medical education. It is remarkable what they have managed to achieve with a fraction of the funding and resources that we are so privileged to have, here in Alberta. The medical school was founded in 1919. The first four students graduated in 1924. Today they graduate 550 doctors per year. They screen 14,000 applicants for 220 positions into the pre-med program. The students do clinical rotations in 23 hospitals with over 7,500 beds. They face a daunting task, as there are estimated to be 5.6 million HIV positive people in South Africa. South Africa, with a population of 55 million, has only nine medical schools. Canada with a population of 37 million has seventeen medical schools. Reference: Dr. Martin Veller
On December 6, 1989, at l’École Polytechnique de Montréal 14 young women were murdered. The government of Canada declared December 6th as The National Day of Remembrance and Action on Violence Against Women.
Things do not seem to have changed. In 2018, 148 women and girls were murdered in Canada. More than 90 per cent of those accused were men. In the majority of cases, they knew the assailant and the intimate partner was implicated 53% of the time.
One in three Canadian women will experience some form of sexual violence in their lifetime. What are we, as physicians doing to reduce the epidemic of violence against women and children? Reference: The first annual report by the Canadian Femicide Observatory for Justice and Accountability
CALENDAR OF EVENTS
ACP Internal Medicine Meeting 2020
April 23-25, 2020
Los Angeles, CA
To save, register by January 31st!
Join your Canadian colleagues in Los Angeles for a complimentary reception hosted by the six ACP Canadian Chapters!
Friday, April 24, 2020 from 6:00-8:00pm
FIRST DRAFT
1230 S. Olive Street
Los Angeles CA 90015
ACP Quebec Chapter Annual Meeting
In collaboration with the Canadian Society of Internal Medicine and ASMIQ
October 14-17, 2020
Quebec City, QC
Information
Rocky Mountain Internal Medicine Meeting/ACP Western Canada Chapters Annual Meeting
November 19-21, 2020
Banff, AB – The Rimrock Hotel
https://www.rockymountainim.com/
@RockyMtnIM
ACP Internal Medicine Meeting 2021
April 29-May 1, 2021
Orlando, FL
ACP Internal Medicine Meeting 2022
April 28-30, 2022
Chicago, IL
PATERNAL ADVICE TO YOUNG INTERNISTS BEGINNING A TEACHING CAREER
(or What I wish I had learned much sooner in my career)
by Dr. Arnie Voth
I have recently retired, at the age of 80, after 40 years of practicing/teaching at the Royal Alex hospital. I look back with many warm memories on a very satisfying career. I have especially cherished my teaching career over these four decades though I confess there were quite a few low points of bad reviews, dysfunctional teams, and times of feeling ‘The 4 weeks are nearly over, and I have accomplished nothing!’ Now is the right time for me to indulge in the octogenarian weakness of giving advice for I will no longer be held to account for failures to follow my advice. What follows is a list of things about bedside teaching I wish I had learned much sooner.
- Learn to shut up! Yes, I am serious. By the time we have acquired that FRCP, we have acquired such a store of knowledge that begs to be passed on to our long-suffering learners. That store of knowledge increases with each year of experience and likewise the temptation to pass it on directly, in long discourses. Sorry, it doesn't work! Long bedside discourses bore learners to death and achieve almost nothing in terms of useful learning. The art of coaching learners to organize their existing knowledge in case discussions in their own words, to ask questions that will fill their own gaps in knowledge and to grow their own approach to building rational problem lists that lead to fruitful investigation and therapy is time consuming and demanding. But it is worth it. The rewards include thoroughly engaged learners, instead of those glazed looks and constant shuffling that say, “O God, when will this be over so I can get on with my work?”, learners who begin to feel and show pride in their clinical thinking and decision making, and best of all, the satisfaction of watching your learners grow their skills day by day instead of just enduring your monologues. So, I repeat: Lesson 1 is learning to shut up and wait for the teaching moment when your expertise is needed for the problem being discussed.
- Learn to know your learners. This lesson took me far too long to learn. As clinician/preceptors, we see our hospital as our second home, our second family, and we accept the daily easy comfort this relationship gives us. It isn't the same for our students and residents. They are shunted from ward to ward, from hospital to hospital, from preceptor to preceptor and so they wrestle daily with a certain subconscious (they are much too busy to give this problem serious thought) alienation that causes a subconscious background of anxiety. Simple things like learning to know and correctly pronounce names, learning at least one or two social facts like hobbies about each learner will mean far more to them than you imagine. If necessary, I would make notes about these simple facts so I could refer to them when needed. I would especially look for shared backgrounds with my team members. Nothing bonds like finding out you shared rural backgrounds, immigrant parents, getting fired from a summer job; what matters is that it is shared. I found that my students and residents rewarded me richly in their enthusiastic participation in work and learning for the few minutes it took to learn something about them.
- In order to teach, you have to be there with your learners. As my hospital slowly transitioned from the old model of individual practices each having a few patients in hospital at a time to the current model of a dedicated teaching team and unit each having from 20 or more patients, many of us tried to keep up our afternoon office practice as we had always done. I quickly discovered that this does not work. It leads to hurried rounds where the preceptor raps out orders as he/she moves rapidly from patient to patient. Once I decided to cancel my office completely, while ‘on service,’ I discovered new vistas in the joys of teaching. I now had the afternoon for proper full reviews of new patients and leisurely reviews of problem patients with the team. I had the time to review and mentor skills like developing effective problem lists (the very bedrock of good internal medicine) and communicating them well in good progress notes. The quality of morning work rounds was greatly improved as my team members could now present well-thought-out plans for their new patients in the morning. Best of all, the team loved these less rushed afternoon discussions, where they felt free to ask any questions and question each other's (including mine) thinking on investigative/diagnostic/therapeutic approaches.
- Trust your Senior Resident. Too often, the senior resident is given too little responsibility. Simply having the senior accompany you as preceptor with an entire team while you rap out orders is a waste of their time and abilities. One of the most effective changes I made in morning work rounds was to split the team in half so the senior would lead one half and I would lead the other half. Then in the afternoon discussions we would brief each other on every active patient. I saw the following benefits:
a. More time for in-depth teaching for both the senior and me. This benefit alone made it worth the effort to manage the change.
b. It gave the senior scope to learn the art of leading work rounds and doing effective bedside teaching.
c. It gave the junior members of the team the benefit of two levels of teaching, each important. As experienced clinicians, we often function automatically as we know the problems so well; so, we don't anticipate questions juniors may have about our rationale for decisions, and they hesitate to ask. The senior resident's memory of these problems and how they resolved them is still fresh and they remember how they approached their learning in specific problems. - Abandon your own notes on patients! I know this is probably the most controversial of my 5 bits of advice. It takes courage. The first morning I came to the ward without anything except my stethoscope, I felt a bit like my first experience at white water canoeing – terror as I looked at the boiling rapids before me. I made the change because my reflections on my teaching told me that I was approaching each patient with my agenda and then waiting for my team members to get to my agenda instead of listening to their approach and concerns. Without my own agenda, I was forced to listen carefully to my team's problem presentations. Now I was hearing the omissions in their presentations, the flawed reasoning, the gaps in their discussions – because I couldn't fill them in from my notes. I think this one change in my methods made more difference to my teaching than any other single change in the last decades of my teaching.
I offer these tidbits of advice to my successors with the hope that they too will enjoy their teaching career as I have enjoyed mine. Next to the gratitude of my patients, the greatest joy in my career has been watching my team members gain new skills and become competent and confident physicians.
EXCELLENT TOOLS AND RESOURCES FOR MEMBERS
- Update your Knowledge with MKSAP 18 Q&A A 54-year-old man is evaluated for a 6-month history of right shoulder pain. He describes the pain as moderately severe aching that is diffusely localized over the shoulder without radiation to the arm. Read more and guess the answer…
- Save 10%, enter code CPDCOVERED2 at checkout before January 31, 2020.
- ACP Journal Club - a summary of the best new evidence for internal medicine from over 120 clinical journals.
- DynaMed Plus®
- ACP JournalWise – searches and filters the most recent articles from the top 120 medical journals.
- ACP Clinical Guidelines
- Annals of Internal Medicine
- IM In-Training Exam - a web-based self-assessment exam for residents to assess their progress.
- ACP advocates for you – Read how...
- Patient Education Tools
- Enhance Your Personal Well-being
ACP AS ADVOCATE
Did you know that the ACP is highly involved in advocacy? Keep up to date with the ACP Advocate Newsletter.
There are many resolutions brought forth for consideration by the Board of Governors. We encourage members to visit www.acponline.org/advocacy and send me your feedback to peter.hamilton@ualberta.ca The Canadian Governors have the opportunity to discuss and vote on resolutions and policy during annual meetings of the Board of Governors.
Visit the Advocacy in Action page for a list of resources and events to help educate and promote action by US policy makers, legislators and others on issues of importance to internists and their patients.
FACP – BECOME ONE TODAY!
- Know a Chapter Member deserving of advancement to Fellowship or Mastership? Nominate them! Or contact me personally at peter.hamilton@ualberta.ca
WELCOME TO NEW MEMBERS
Luc A Benoit, MD
Sana Vahidy, MD
Aditi Amin, MD
Archana Vijay, MBBS
Gabriel Fabreau, MD
Subrata Datta, MBBS
Ayodele Adebayo, MD
Brian Buchanan, MD
GET INVOLVED IN YOUR CHAPTER!
Be an active part of this chapter! There are many volunteer opportunities on various committees – email me at peter.hamilton@ualberta.ca
Follow the ACP Canadian Chapters on Twitter! @ACPCanadian

