Choosing Your Path: Lung Transplant Medicine, Pulmonary and Critical Care Medicine
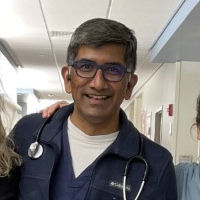
Satish Chandrashekaran, MD, FACP, FCCP
Clinical Assistant Professor of Medicine
Lung Transplant Fellowship Program Director
Division of Pulmonary and Critical Care and Sleep Medicine
University of Florida, Gainesville, Florida
Residency training: St Francis Hospital, Evanston, IL.
Fellowship training: Critical Care Medicine, Mayo Clinic Rochester, MN
Pulmonary Medicine, Mayo Clinic, Jacksonville, FL
Practice setting (e.g., academia, hospital or health system, private practice): I work in a university hospital. This is an academic setting with various residency and fellowship training programs. My clinical assignment varies every week among lung transplant ICU, transplant floor, bronchoscopy, and clinics.
I evaluate patients with end-stage lung disease (like COPD, pulmonary fibrosis, cystic fibrosis) who have exhausted all medical therapies. I assess these patients in the clinics and determine if they are potential lung transplant candidates. If there are no apparent contraindications, the patients are placed on the waitlist for organ transplantation. Once a suitable donor is available, the transplantation surgery is performed by the thoracic surgeon. I take over the patient's care once the patient arrives in the ICU from the operating room after the transplantation surgery. After the patient is liberated from the mechanical ventilator and in some cases from an ECMO machine (extracorporeal membrane oxygenation machine, which functions as an artificial lung machine), the patient is transferred to the floor. I take care of this patient on the floor and adjust their immunosuppression to prevent rejection of the lungs. I perform periodic bronchoscopy and obtain tissue biopsies to detect rejection at a very early stage. Upon discharge from the hospital, I frequently see these patients to adjust medications and follow the lung function. Hence, I am involved in the management at every stage, from their initial evaluation to post-transplant follow-up.
Years in practice: 7 years as a hospitalist/internal medicine. 7 years as a lung transplant physician.

How many patients do you see daily? I am involved in the clinical care of about 20 patients daily when I am rounding in the lung transplant ICU. When I rotate on the lung transplant floor, I care for 20–25 lung transplant patients. When I am in the clinic, I see about 14–17 patients daily. I have one fellow and an advanced nurse practitioner who help me in these patients' clinical care in the ICU, the floor, or clinic settings.
In a given week, what nonclinical duties do you have outside of patient care? In addition to being a clinician, I am also the lung transplant fellowship program director. My focus is to train the next generation of well-rounded lung transplant physicians. Applicants for this fellowship include physicians who have completed a 3-year pulmonary critical care fellowship. This fellowship is a 1-year training in advanced lung failure and transplantation. There are only a half dozen programs in the country that offer this training, though there are 60 lung transplant centers. There is a dire need for well-trained lung transplant physicians in the country. The UF lung transplant fellowship provides very comprehensive training in this field.
The most challenging and rewarding aspects of caring for patients in your specialty or subspecialty: As a pulmonary critical care and lung transplant physician, I see some of the sickest patients in the hospital. These include patients who have exhausted medical therapy for their end-stage lung disease and are on mechanical ventilation and at times an artificial lung machine (ECMO). In some cases, we can rescue these patients with lung transplantation. Many of them can return to their everyday lives. This is extremely rewarding.
On the other hand, I also take care of patients who have multiorgan failure, and lung transplant alone would not fix it. In cases like these, I initiate end-of-life discussions and transition them to palliative care/hospice, which is challenging and emotionally draining. The past year has been difficult for all frontline workers, including nurses, respiratory therapists, ER physicians, and ICU doctors. We all have witnessed the loss of many patients, which is heartbreaking. But I am grateful to this community that has stood up to this challenge.
What is the most important clinical skill in your daily practice? Bronchoscopy with transbronchial biopsies is one of the essential clinical skills in my daily practice.
What characteristics, or personal qualities, help you most in your specialty/subspecialty (e.g., being unafraid to ask probing questions)? I have realized from my last 20 years of practice that the most important quality that the patients appreciate in a physician is honesty. No matter how difficult or complicated the information is, I make every effort to be honest with the patient and their family. I encourage patients and their families to ask questions. This helps me to determine their insight into their health care situation.
How do you feel about the balance of your professional and personal lives? After the fellowship, my initial years were rather intense professionally as I tried to establish a lung transplant program. At this point, I have six other associates, and I have cut back to achieve a balance in my professional, academic, and personal life.
Advice for diverse medical trainees in your specialty/subspecialty: There is a high need for well-trained internal medicine– and subspecialty-trained physicians in the United States, and the demand appears to be growing every year. Moreover, the current pandemic has unmasked the health care inequities and deficiencies in our system. I strongly encourage and support diverse medical students and fellows to pursue training in internal medicine and subspecialties. There is a dire need for pulmonary critical care and lung transplant physicians in the country. I am convinced that you will be able to touch these patients' lives and be instrumental in bringing about changes that would address health care inequities.
What resources do you suggest for trainees interested in your specialty/subspecialty (books, podcasts, articles, websites)? The American Thoracic society has some information in their career development section.
What is your motto, or favorite saying, to describe your life in this specialty? "No one cares how much you know, until they know how much you care"—Theodore Roosevelt
No matter how many degrees we earn or how many fellowships we complete or how many research papers we publish, we remain the doctor for the patient. Every patient deserves to be treated with respect and empathy. Be honest. These qualities will enable a physician to build a strong relationship with the patient and win their trust. We always need to put the needs of the patient first.

