Medicare’s Quality Payment Program (QPP)
What's New
Making Care Primary
On June 8, 2023, CMS announced a new voluntary primary care model, Making Care Primary (MCP) which will launch on July 1, 2024. The MCP model provides primary care clinicians with enhanced payments, tools, and support to improve the health outcomes of their patients and aims to ensure that patients receive care to meet their health goals and social needs. The MCP model’s three tracks support building infrastructure, implementing advanced primary care, and optimizing care and partnerships; they are designed to recognize participants’ varying experiences in value-based care. This model will operate in eight states, Colorado, Massachusetts, Minnesota, New Mexico, New Jersey, New York, North Carolina, and Washington. Read ACP’s summary of the MCP model and statement on how it incorporates some of the key elements that ACP proposed in the Medical Home Neighborhood model that we submitted for consideration to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) and ultimately approved by HHS. In response to the COVID-19 pandemic and the ACP’s advocacy, CMS extended the MIPS extreme and uncontrollable circumstances exception. Applications for the 2023 performance year are due January 2, 2024. Find more information here.
CMS published the 2024 Medicare Physician Fee Schedule/QPP Final Rule on November 2, 2023. Read ACP's detailed summary (ACP Member login required) and comments on the 2024 PFS final rule.
MIPS
Merit-Based Incentive Payment System
The Merit-Based Incentive Payment System (MIPS) adjusts payments based on a clinician's performance across 4 categories: Quality (30%), Promoting Interoperability (25%), Improvement Activities (15%), and Cost (30%). Learn more
APMs
Alternative Payment Models
APMs structure payment to incentivize quality and value. Clinicians who participate in certain “Advanced APMs” that satisfy advanced risk, quality, and technology requirements may be excluded from MIPS and eligible for a 5% Medicare bonus. Learn more
Other Value-Based Payment Reform Efforts
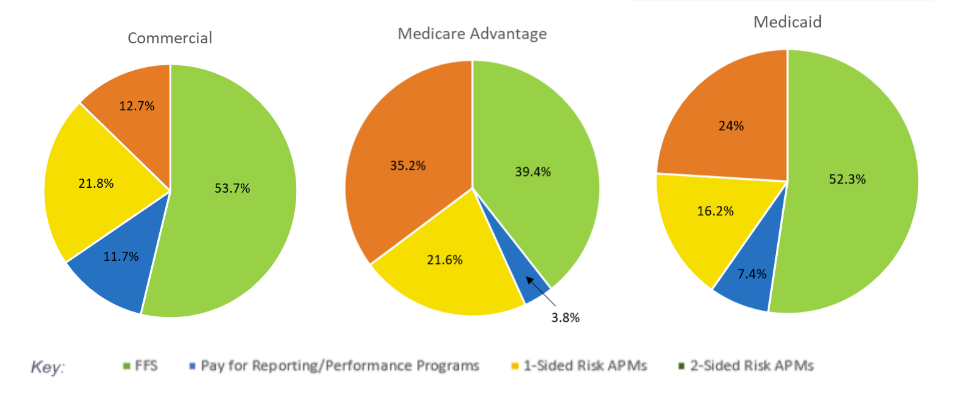
Medicaid, Medicare Advantage, and private payers have increasingly been developing their own quality performance programs and APMs. To the right is the breakdown of value-based payments for commercial, Medicaid Advantage, and Medicaid payers, based on 2022 data.
Source: Health Care Payment Learning & Action Network
ACP Advocacy
- ACP Comments on 2024 Medicare Physician Fee Schedule and Quality Payment Program Final Rule
- ACP Comments on Proposed 2024 Physician Fee Schedule, Medicare Shared Savings Program, and Quality Payment Program Rule
- ACP Summary of Proposed 2024 Physician Fee Schedule, Medicare Shared Savings Program, and Quality Payment Program Rule (ACP Member Exclusive)
For more information or questions or concerns regarding specific QPP/MACRA-related issues, email policy-regs@acponline.org.

