This toolkit shares best practices and real-life examples of successful team-based clinical care models that include internal medicine physicians working with Nurse Practitioners (NPs) and Physician Assistants (PAs) and other members of the clinical care team. The resources below can help you foster productive and purposeful internal medicine teams.
Table of Contents
- Why Should We Practice in Teams?
- What Is Team-Based Care?
- Steps to Optimal Team-Based Care Framework
- Learn More About NP’s and PA’s
- Case Studies and Real-life Models of Team-Based Care
- Adding an NP or PA to Your Practice
- Utilize and Train Existing Team Members
- Partnering in Team-Based Care with Patients
- Change Management and Sustainable Teams
- 5 Quick Wins for Team-Based Care
Why Should We Practice in Teams?
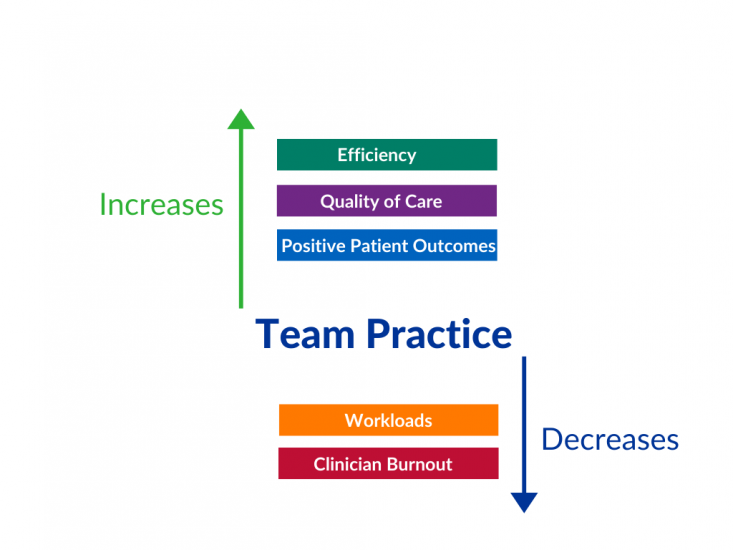
High functioning clinical teams are essential for the delivery of high value healthcare and have been associated with:
- Decreased workloads
- Increased efficiency
- Improved quality of care
- Improved patient outcomes
- Decreased clinician burnout/turnover
Source: Implementing Optimal Team-Based Care to Reduce Clinician Burnout – from the National Academy of Medicine
What Is Team-Based Care?
A team-based model of care strives to meet patient needs and preferences by actively engaging patients as full participants in their care, while encouraging and supporting all health care professionals to function to the full extent of their education, certification, and licensure.
Actively engaging patients as full participants in their care, while encouraging and supporting all health care professionals to function to the full extent of their education, certification, and licensure.
- Health care teams are defined as two or more health care professionals who work collaboratively with patients and their caregivers to accomplish shared goals. For example, an internist and an NP working together to transition a patient with diabetes to insulin therapy.
- A health care team may involve a wide range of team members in various settings. For example, a small ambulatory health care team may include an internist and medical assistant working together to improve the rates of influenza vaccination in their practice. A large inpatient team might include a nurse case manager, social worker, clinical pharmacist, physician assistant, several medical residents, several medical students, an attending physician and unit nurse manager meeting daily to run the list of patients on a floor.
- Potential members include physicians, nurse practitioners and physician assistants, medical assistants, pharmacists, social workers, trainees, patients and their families, and others identified as persons necessary to help achieve shared goals.
Resources
Access these resources to help you define the team and understand general principals behind team-based care:
- Cambridge Health Alliance Model of Team-Based Care Implementation Guide and Toolkit - The Cambridge Health Alliance Model of Team-Based Care Implementation Guide and Toolkit provides information and resources on team-based care, the role of each team member, and sample huddle strategies.
- Creating Patient-centered Team-based Primary Care – A proposed blueprint for patient-centered team-based care and strategies to provide patient-centered team-based care.
Steps to Optimal Team-Based Care Framework
- Foster mutual trust and physical and psychological safety
- Clarify roles and expectations
- Practice effective communication
- Track a set of shared measurable goals

Resources
Access these resources to help build this framework and ensure clinical and administrative systems support team members in their defined work:
- IOM Core Principles & Values of Effective Team-Based Health Care – This discussion paper presents basic principles and personal values that characterize interprofessional team-based care. Developed by individual participants from the IOM’s Best Practices Innovation Collaborative, the authors identified key findings from health care literature, and used interviews with eleven teams located across the United States to clarify how these factors shape effective team-based care.
- Team-Based Care – This module from the AMA Steps Forward explores how to improve patient care and team engagement through collaboration and streamlined processes. It will help you define elements that constitute the model of team-based care, describe how to implement team-based care in your practice, and identify benefits of implementing team-based care in your practice.
- Advancing Team Culture: Workforce Effectiveness During COVID-19 and Beyond – This playbook from Vizient sheds light on significant developments in clinical teamwork during 2020 and shares proven strategies for fostering effective teams.
- Implementing High-Quality Primary Care: Rebuilding the Foundation of Healthcare – Chapter 6 of this report from the National Academy of Medicine, entitled “Designing Interprofessional Teams and Preparing the Future Primary Care Workforce”, focuses on key design elements of interprofessional teams and highlights the roles that extended care team members can play in delivering high-quality primary care.
Learn More About NPs and PAs
The term 'Advanced Practice Providers' refers to both Physician Assistants and Nurse Practitioners.
An improved understanding of the various roles, training requirements, and scope of work may help internists who are interested in building, expanding, or improving team-based care in their practices. The term “Advanced Practice Providers” refers to both Physician Assistants and Nurse Practitioners. NPs and PAs have very different requirements for both basic science education and clinical experience. In addition, their scope of practice and integration into the healthcare workforce varies significantly by state.
Resources
The resources below may help you with your decision to add an NP or PA to your team or more effectively incorporate the APP’s on your team:
- NPs vs PAs; What’s the Difference? - This short article summarizes how NPs and PAs are alike and how they are different. It covers differences in the focus of their education, certification and licensure, and in state law mandating physician involvement in practice. It even includes a handy set of key questions to ask prior to hiring an APP.
- PAs & NPs: Similarities and Differences – This infographic presents the similarities and differences between NPs and PAs in an easy-to-read infographic.
- Physician Assistant Scope of Practice - This state law chart from the AMA outlines several aspects of state laws regulating physician assistant practice including prescriptive authority, requirements for collaborative or supervisory arrangements, regulation, and scope of practice determination.
- PA Scope of Practice – This resource from the AAPA explains more about the scope of practice of PAs.
- Nurse Practitioner Practice Authority – This state law chart from the AMA outlines nurse practitioner practice authority by state.
- PAs and Team Practice - This resource from the AAPA highlights the important role of PAs in team practice.
Case Studies and Real-life Models of Team-Based Care
Real-life examples of successful team-based care in Internal Medicine showcase ways in which team-based care involving nurse practitioners, physician assistants, pharmacists, and others are working together with patients and caregivers in both inpatient and outpatient settings.
Outpatient
- Clinician Well-Being at Virginia Mason Kirkland Medical Center: A Case Study - This case study provides an overview of initiatives that support well-being and reduce burnout in clinicians who work at the Virginia Mason Kirkland Medical Center. The purpose of this case study is to provide readers with tangible information to understand how Kirkland Medical Center has adopted programs and policies that support wellbeing. These include allowing clinicians to practice to the full extent of their education and training and standardizing roles for medical assistants.
- Building Teams in Primary Care: 15 Case Studies – This set of case studies explore a variety of practices who successfully implemented teams. Case 11 (page 36-40) specifically addresses the use of physician assistants and nurse practitioners into Harvard Vanguard Medical Associates, a large multi-specialty group practice in the Boston metropolitan area, to successfully manage chronic conditions.
- Watch this 3-minute video that describes how they have implemented effective team based primary care at Emory Patient Centered Primary Care.
- Team-Based Care – This TCPi Team-Based Care power pack highlights Union Square Family Health Center, a Family Medicine site of the Cambridge Health Alliance in Boston, MA and how they successfully implemented a team-based care model as a sustainable solution to overwork.
Inpatient
- Video on Interdisciplinary Rounds – This video features a patient care team at Christiana Care's Wilmington Hospital intensive care unit that demonstrates the patient and family centered care practice of interdisciplinary rounds at the bedside.
- Leveraging Advanced Practice Providers during a Crisis: Lessons Learned from Top Healthcare Systems – This white paper from the American College of Healthcare Executives shares crisis strategies from APP leadership across the nation during the COVID-19 pandemic and showcases the innovative ways APPs met unprecedented demands.
- Integrating Advanced Practice Providers into value based care strategies: One organization’s journey to achieve success through interprofessional collaboration – This case study from the Journal of Interprofessional Education and Practice showcases an urban academic pediatric hospital that enhanced the use of Advanced Practice Providers (APPs) to optimize care.
Adding an NP or PA to Your Practice
During the hiring process, defining team members’ roles can help you empower your team. Oversight and management of a team of advance practice providers is also essential to a highly functioning team.
Resources
These job descriptions and other hiring resources can help you facilitate decisions about which patients see which team members, and the best ways to optimize outcomes while having everyone work at the top of their scope.
- The Business Case for Hiring a Nurse Practitioner – this article outlines estimated expenses, potential revenue generation and potential profits to expect after the addition of an NP to your practice.
- Sample APRN Job Description – Sample APRN job description for an outpatient internal medicine clinic.
- Sample Physician Assistant Job Description – Sample PA job description for an inpatient setting.
- Sample Core and Specialty Privileges for PAs – Resource from the AAPA.
- PAs: Credentialing, Privileging, and Assessing Competency (FPPE & OPPE) – Resource from the AAPA.
- Third-Party Reimbursement for PAs – Resource from the AAPA.
- Strategies for Recruiting NPs and PAs - In this article from the ACP Hospitalist, two hospitalists share their program’s model for outreach, screening, and interviews.
Utilize and Train Existing Team Members
Hiring new staff is not always necessary to make the most of team-based care. By compensating and valuing the team you already have in place, you can decrease staff turnover and make more a more successful practice.
- Remember the importance of the front desk staff and their role on the team
- Medical assistants are often overlooked but crucial members of the team
- Standardize work processes
- Engage all team members in workflow redesign to get buy in and assure that the new process makes sense
- Some examples: standing orders for influenza vaccination during flu season increase rates of vaccination without need for physician involvement; MA’s and LPN’s take patient portal review shifts to decrease response time and clinician burden; uptrain MA’s to scribe encounters in the EHR so that clinicians can focus on patient centered communication and clinical decision making
- Clarify roles
Partnering in Team-Based Care with Patients
Patients, families, and other caregivers need a clear understanding of the roles of the interprofessional care team with explanations of which role will serve which purpose in their care. The health care team should provide information to patients, families, and other caregivers so they can make informed healthcare decisions in partnership with their care team.
Resources
The following resources can help patients understand the different roles that make up the interprofessional health care team and how they might interact with each:
- Who’s Who on the Healthcare Team: An Interdisciplinary Approach - This article provides a brief introduction to the educational background and role of the different professionals a patient might typically encounter in a hospital.
- Your Health Care Team - This article provides a brief description of the roles of the different professionals a patient might typically encounter in a hospital.
- Your PA Can Handle It – This patient-facing resource explains more about the physician assistant role on the healthcare team.
Change Management and Sustainable Teams
Physicians, clinicians, non-clinical staff and patients may have some difficulty adapting to team-based care models. Change management principles may ease adoption by stakeholders and help sustain the team and its members over the long term. Ongoing, structured communication and feedback are essential to optimize team performance and help to sustain teams over time. Relatedness and the ability for team members to enjoy each other’s company at work should be nurtured and encouraged. High functioning teams have been associated with reduced clinician burnout and improved patient outcomes.
Resources
These resources address how team-based care can reduce burnout and how to sustain team-based care models in the long term.
- ACP’s Well-being and Professional Fulfillment Resources – These resources from ACP can help physicians and their teams reduce burnout and find ways to enhance professional satisfaction and wellbeing.
- Team-based Care and Flexible, Adaptable Leadership - This menu of recommendations can help you get started with developing a plan for effective team-based communication and leadership in your practice.
- Physician Assistant Burnout Resources – These resources from the AAPA help support the well-being and professional satisfaction of physician assistants.
- Mini but Mighty Appreciative Inquiry – Appreciative Inquiry is an organizational development model that takes a positive approach to systems change. This webinar, developed by Kerri Palamara, MD, FACP, Director of the Center for Physician Well-being at Massachusetts General Hospital and Physician Coaching Services Lead for ACP, and presented by North Carolina Well-being Champion Marion McCrary, MD, FACP, guides you through using the AI approach in your practice and teaching others to do the same.
5 Quick Wins for Team-Based Care
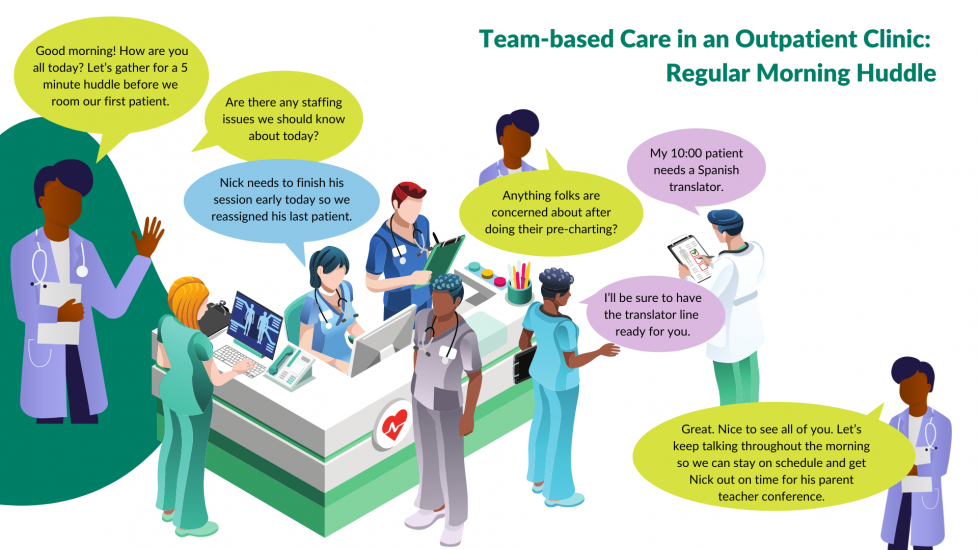
To put the Steps to Optimal Team-Base Care into action, here are five easy-to-implement examples that any care team can put into place:
1. Hang pictures of team members on the wall
2. Invite patients/families to join the clinical team
Both help foster mutual trust and physical and psychological safety
3. Hang a ribbon from each staff person’s badge that states their role
4. Include team members and their roles into the new patient visit
Both help clarify roles and expectations
5. Start each clinical session with a short team huddle
Emphasizes the practice of effective communication
These ideas help to enhance team-based care by optimizing the team you already have, and working with intention to involve everyone consistently on the care team.

