
October 2011
- Feature: Following Your True Path: An Interview with Timothy McCall, MD, General Internist and Yogi
- Medical Student Perspectives: Navigating the Daunting Challenge of Research
- My Kind of Medicine: Matthew L. Nathan, MC, USN, FACP, FACHE
- Nominate your Favorite Internist to be featured in My Kind of Medicine
- Internal Medicine Interest Group of the Month: University of Texas-Houston
- Submit Your IMIG for Internal Medicine Interest Group of the Month
- Ask the Program Director: Personal Statements
- Advocacy Update: NHSC Announces Students to Service Loan Repayment Pilot Program
- Winning Abstracts: Effect of Palliative Care Services on End of Life Care in Cancer Patients
- Subspecialty Careers: Hospice and Palliative Medicine
- In the Clinic: Colorectal Cancer Screening
- Virtual Dx - Interpretive Challenges from ACP
- Highlights from ACP Internist® & ACP Hospitalist®
Feature: Following Your True Path: An Interview with Timothy McCall, MD, General Internist and Yogi
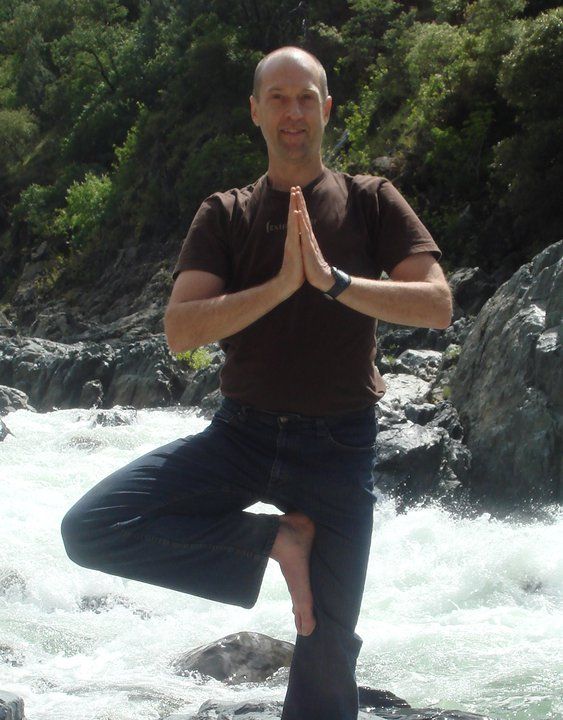 While many general internists practice hospital or
office-based medicine, the wealth of knowledge and experience that
comes with this training can take you to lots of interesting
places. Dr. Timothy McCall, Medical Editor of the Yoga Journal,
shared his path from being an office-based primary care provider to
an award-winning author and internationally-recognized Yoga
Healer.
While many general internists practice hospital or
office-based medicine, the wealth of knowledge and experience that
comes with this training can take you to lots of interesting
places. Dr. Timothy McCall, Medical Editor of the Yoga Journal,
shared his path from being an office-based primary care provider to
an award-winning author and internationally-recognized Yoga
Healer.
Medical Student Perspectives: Navigating the Daunting Challenge of Research
What are your thoughts when you hear the subject research? Are you thinking, how in the world can I fit research into my already busy schedule? Maybe you are thinking, I want to start some research, but I just don't know where to begin? Maybe you are in the middle of a research project and wishing you had chosen a different project, a different mentor, or a different field of research.
MoreMy Kind of Medicine: Real Lives of Practicing Internists: Matthew L. Nathan, MC, USN, FACP, FACHE

Dr. Nathan - a Rear Admiral in the United States Navy -decided on a career as a physician because of a personal experience.
"My desire in becoming a physician was cemented when I watched my mother battle a terminal illness. I was in college at the time, and I carefully watched all the physicians who participated in her care. I saw how they artfully weaved together science and compassion to provide my mother with the care she needed. After this experience, I knew that I wanted to become a physician."
MoreNominate your Favorite Internist to be Featured in My Kind of Medicine
Do you have a favorite internist? Maybe a program director who has inspired you? Or maybe just a doctor with fascinating story?
Nominate an internist today!
Internal Medicine Interest Group of the Month: University of Texas - Houston
The new 2011-2012 officers for AIMS (Association of Internal Medicine Students) at UT-Houston in the Texas Medical Center have collectively implemented the goal for our IMIG to be more active and hands-on than previous years, as well as to better involve our 3rd- and 4th-year members. To tackle this undertaking, September became a busy month for AIMS.
MoreSubmit Your IMIG for Internal Medicine Interest Group of the Month
Do you think your IMIG has what it takes to be featured as the "Internal Medicine Interest Group of the Month" in an upcoming issue of IMpact? Deadline for submissions is November 1.
MoreAsk the Program Director: Personal Statements

How important is the personal statement when making your decision about a candidate for an interview? I have confidence I can write a perfectly acceptable personal statement, but probably not one that can really "wow" the reader. I'd much rather rely on my CV and interview skills to get ranked, but if a superb personal statement is needed I'd like to know now.
See what six different Program Directors have to say!
Advocacy Update: NHSC Announces Students to Service Loan Repayment Pilot Program
The National Health Service Corps (NHSC) Students to Service Loan Repayment Program (S2S LRP) will provide loan repayment assistance to medical students (MD and DO) in their last year of school in return for serving in eligible Health Professional Shortage Areas (HPSAs) of greatest need.
MoreWinning Abstracts from the 2011 Medical Student Abstract Competition: Effect of Palliative Care Services on End of Life Care in Cancer Patients
End-of-life (EOL) cancer care affects a large number of Americans each year. Terminal cancer patients have been experiencing increasing use of overly aggressive anticancer treatments and disparities in access to hospice services.
MoreSubspecialty Careers: Hospice and Palliative Medicine
Palliative medicine aims to relieve symptoms and pain a patient suffers due to a serious illness. While hospice care is provided for patients facing a terminal diagnosis who no longer wish to undergo curative treatment.
MoreIn the Clinic: Colorectal Cancer Screening
Colorectal cancer is the fourth most common type of cancer and the second leading cause of cancer death in the United States (1). Outside the United States, the impact of colorectal cancer is also immense. In terms of global incidence, it ranks third among cancers affecting women and fourth for men (2).
In the Clinic is a monthly feature in Annals of Internal Medicine that focuses on practical management of patients with common clinical conditions. It offers evidence-based answers to frequently asked questions about screening, prevention, diagnosis, therapy, and patient education and provides physicians with tools to improve the quality of care. Many internal medicine clerkship directors recommend this series of articles for students on the internal medicine ambulatory rotation.
Virtual Dx - Interpretive Challenges from ACP

Which of the following is the most likely diagnosis?
AnswerHighlights from ACP Internist® & ACP Hospitalist®
Sports
internists treat players as patients
These internists turned their own athletic pursuits into careers
for professional sports teams, treating high-caliber athletes as
they practice and play. When working the sidelines, it's just
another day not at the office.
Managing the
elderly with cardiovascular disease
As patients are living longer, they're seeking more care for their
cardiovascular diseases, as well as the accompanying comorbidities
such as diabetes. Effective therapy is possible in the older
population, say the experts.
Newman's
Notions: The wisdom of teens
Our editorial advisor learns a thing or two about diagnosis from an
unusual source: his teenage son.
Tapped
out: Drug shortages send hospitalists scrambling
The drugs in limited or non-existent supply can vary across the
country, but the number of medications affected has steadily
increased, in some cases undermining patient care.

